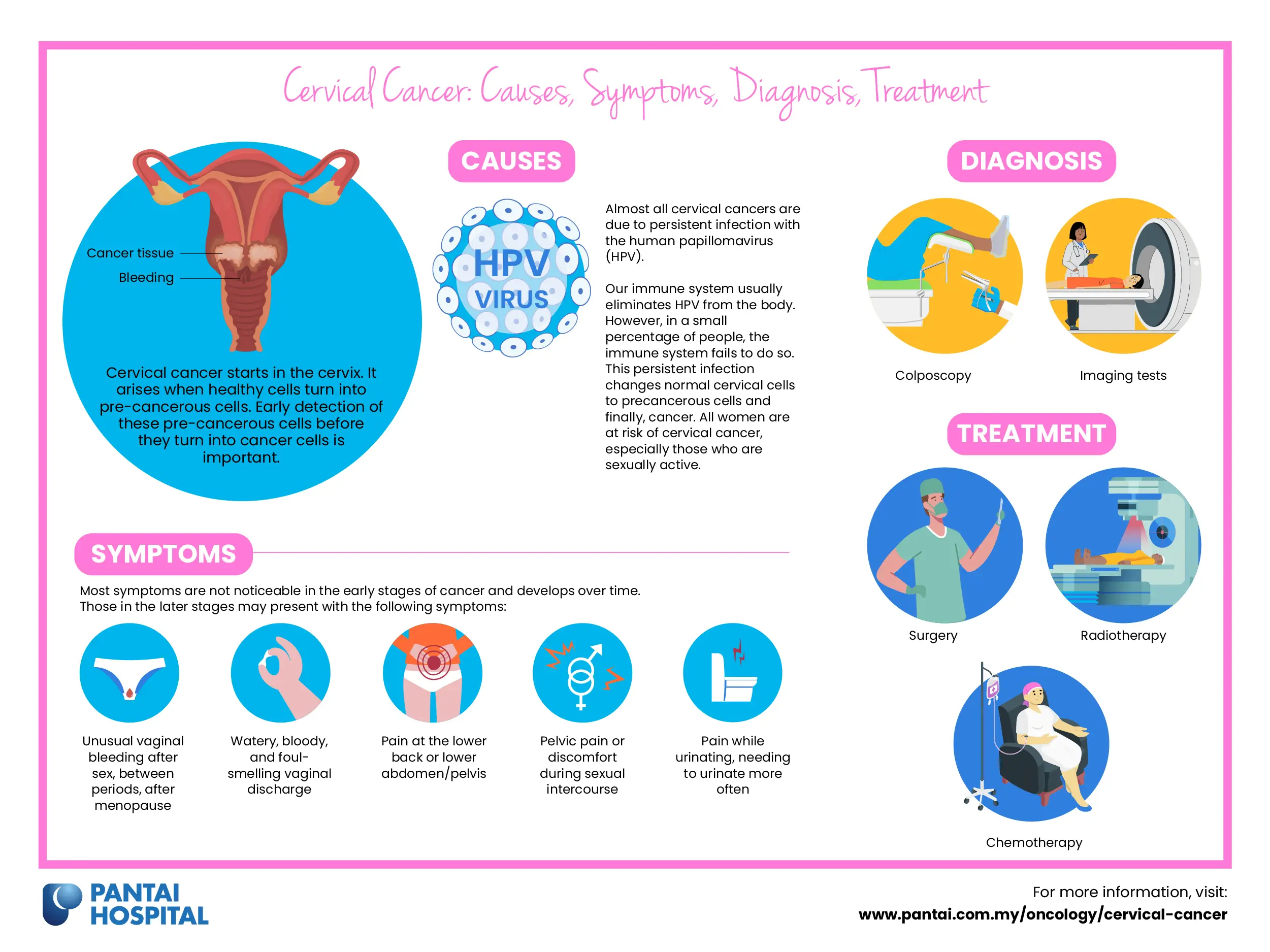
Cervical cancer starts in the cervix (the opening between the uterus and the vagina). It arises when healthy cells turn into pre-cancerous cells. Therefore, the early detection of these pre-cancerous cells before they turn into cancer cells is important.
Cervical cancer is one of the most prevalent cancers among Malaysian women and it typically affects women between the ages of 14 to 44 years.
Cervical cancer occurs in the cervix or birth canal cells, which connect the uterus and the vagina. There are two types of cervical cancers, squamous cell carcinoma and adenocarcinoma. These are determined by the appearance of cells under a microscope.
Almost all cervical cancers are due to persistent infection with the human papillomavirus (HPV).
Our immune system usually eliminates HPV from the body. However, in a small percentage of people, the immune system fails to do so. This persistent infection changes normal cervical cells to precancerous cells and finally, cancer. All women are at risk of cervical cancer, especially those who are sexually active.
There are 14 high-risk HPV subtypes which can lead to the predisposition of cervical cancer. Infection with HPV, especially with HPV types 16 and 18, increases the risk of cervical cancer. The majority of HPV infections result from both penetrative sexual intercourse and non-penetrative sexual activity.
HPV infections typically do not cause physical symptoms. However, in certain individuals, these infections may lead to pre-cancerous lesions that if left untreated, can develop into cancers of the anus, cervix, vulva, and vagina in women.
The following factors increase the risk of developing cervical cancer:
Most symptoms are not noticeable in the early stages of cancer and develops over time.
Those in the later stages may present with the following symptoms:
These symptoms can be caused by numerous other conditions, which are more common than cervical cancer. Therefore, Therefore, it is highly recommended for all women to routinely go for their screening test and consult a gynaecologist if you notice one or more of these symptoms.
Your doctor would initially inquire about your general health and symptoms before conducting thorough physical and gynaecological tests. You may also require blood and urine tests.
Other diagnostic tests may include:
Learn more about the different types of screening and diagnostic procedures performed to diagnose cervical cancer.
The course of treatment for cervical cancer is determined by stage and type of cancer. Key treatments include surgery, chemotherapy and radiotherapy.
Surgery is typically the main treatment method used if the cancer is detected early. The surgeries used in the treatment of cervical cancer include:
Radiotherapy employs high-energy radiation to reduce the size of tumours and kill cancer cells. This procedure is used to alleviate the symptoms of advanced cancer. Radiotherapy may be used as the main method of treatment if the tumour is large or has spread.
There are two types of radiotherapy:
Chemotherapy is a cancer treatment that involves intravenous administration of cytotoxic drugs via blood vessels for systemic circulation.
Learn more about the different types of treatment technologies to treat cervical cancer.
Vaccination and regular screening tests are the best ways to prevent cervical cancer.
Early detection of cervical cancer occurs in nearly half of the cases, making it highly treatable. Therefore, the majority of women should be routinely screened for cervical cancer via a HPV test, Pap test, or a combination of the two. Women should be routinely screened once every few years once they turn 21.
Consult your doctor to determine if you would benefit from a cervical cancer screening.
Early detection of cervical cancer makes it easier to treat the disease with effective and appropriate treatment. A dedicated multidisciplinary team of specialists and oncologists at Pantai Hospitals is available for consultation to provide the best care and assistance to patients through screening, diagnosis, and treatment.
Get in touch with us to book an appointment today if you have any concerns or questions about cervical cancer treatment options.
Pantai Hospitals have been accredited by the Malaysian Society for Quality in Health (MSQH) for its commitment to patient safety and service quality.